Abstract
Background- High molecular weight Kininogen (HK) is a nonenzymatic co-factor of the contact activation system. HK binds prekallikrein (PK) and FXI to surfaces in proximity to FXII, amplifying PK activation by FXIIa and the reciprocal activation of FXII by activated PK (PKa), as well as FXI activation of FXIIa. PKa cleavage of HK also liberates bradykinin-a proinflammatory and vasoactive nanopeptide. The aim of this study was to define the pro-thrombotic role of kininogen in venous thrombosis (VT) and to use in vivo serial analysis of thrombus development to understand the recruitment and retention of platelets in the growing thrombus in the absence and presence of kininogen.
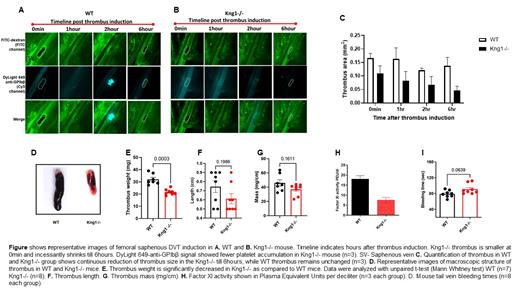
Methods- The development of VT in mice deficient in kininogen (mKng1-/-) was compared to that in their wild-type littermates. A femoral-saphenous stasis VT model was prepared by ligating both saphenous and femoral veins. Next VT formation, growth, and dissolution (n=3 for each group) was monitored using intravital microscopy (IVM) via a multichannel epifluorescence microscope (Nikon Eclipse 90i). To induce stasis VT, FITC-dextran (10 mg/kg, ex/em 488/520 nm) was injected retro-orbitally, and then continuous light irradiation (20x objective, 475nm/35nm) of the saphenous vein was applied for 5 minutes. FITC-dextran fluorescence angiography monitored thrombus formation and dissolution. Immediately after VT formation, platelet accumulation at the thrombus site was monitored in the Cy5 channel (630/38 nm) via injection of a GPIbβ antibody conjugated with Dylight-649 (150nmol/kg), over time. All images were identically windowed in each channel, and thrombus area was measured using NIH ImageJ software. To corroborate IVM studies, we also evaluated a complete stasis model of inferior vena cava (IVC) ligation (n=7-8 per group). Thrombi were harvested after 48 hours and thrombus weight and length were measured to estimate thrombus mass. FXI circulates in blood as a homodimer along with HK. We determined the effect of kininogen deficiency on FXI activity. FXI activity assay used a combination of inhibitors, serially, to monitor the cleavage of substrate specific to activated FXI and release of chromogen, as a function of FXI activity. Finally, to determine the effects of Kng1 deficiency on bleeding, tail vein bleeding times were also determined (n=8 per group).
Results- In femoral-saphenous stasis VT, thrombus developed in both groups immediately following FITC-channel light irradiation. However, thrombus size was smaller in Kng1-/- as compared to WT (Figure 1). Results from serial IVM of VT indicated faster thrombus dissolution in the Kng1-/- group. Lower platelet signals, as shown at 2 and 6 hours in the Kng1-/- mice may be consistent with this hypothesis. Thrombus area analysis suggested decreased thrombus formation in the Kng1-/- animals, and temporal analysis indicated faster dissolution by 6 hours (Figure 2). IVC ligation results corroborated the findings of femoral-saphenous DVT model, demonstrating that thrombus weight was significantly lower in Kng1-/- mice as compared to WT (p<0.001, Figure 3). FXI activity was also decreased in the Kng1-/- group (p<0.10). Tail vein bleeding times, however, showed no increased bleeding in Kng1-/- mice.
Conclusion- These initial results suggest a pro-thrombotic role of kininogen and a protective role of kininogen deficiency in two murine venous thrombosis models, without incurring a bleeding penalty. Thrombus dissolution was faster and platelet accumulation was inhibited in Kng1-/- mice. These findings suggest that targeting kininogen may provide a new approach to prevent and treat venous thrombosis.
McCrae: Dova, Novartis, Rigel, and Sanofi Genzyme: Consultancy; Sanofi, Novartis, Alexion, and Johnson & Johnson: Consultancy, Honoraria. Jaffer: Mercator, Inc.: Other: Sponsred research.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal